Fighting the National Opioid Epidemic
Innovations & Initiatives
08/07/2018
How Centene developed OpiEnd™ to help those most at risk
In an effort to combat the wide-ranging opioid epidemic affecting communities across urban, suburban, and rural areas, Centene and more than a dozen other health insurance companies launched a task force in 2017. Aligned with Centene's commitment to saving lives and improving outcomes, the task force pledged to fight the opioid epidemic through quality enhancements and improved access to addiction treatment.
To support Centene's membership and our communities against the scourge of addiction, Centene's clinical leadership developed the comprehensive OpiEndTM program. OpiEnd utilizes Centene's proprietary business intelligence tools to identify at-risk members for potential opioid misuse. This proactive approach employs early intervention to prevent opioid misuse and, ultimately, to save lives, one member at a time.
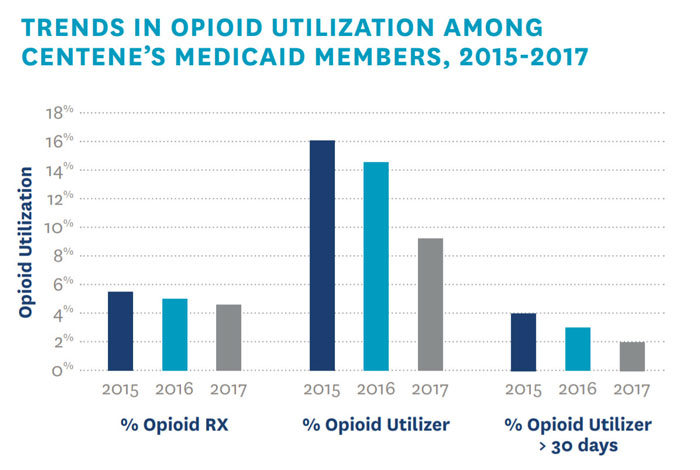
Additionally, the OpiEnd Pharmacy Advisory Group established a pharmacy opioid policy designed to prevent opioid misuse by restricting the daily dosage and maximum days of use prescribed for members. OpiEnd has trended toward positive results, specifically among Centene's Medicaid members. In 2017, OpiEnd observed a trend toward a decrease in the percent of opioid prescriptions, opioid utilizers, and those utilizing opioids for more than 30 days.
Centene encourages local innovation, and state health plans offer grassroots perspectives on the fight against opioid addiction. Plans often host forums for healthcare professionals and community leaders to connect, engage, and identify solutions to the crisis, among other activities. Centene's Sunshine Health plan recently developed an online provider toolkit and presented free online courses to help providers identify the best ways to prevent opioid misuse and addiction.
Centene's comprehensive strategy to address the national opioid epidemic is an example of how the company uses technology, innovation, and collaborative partnerships to improve the quality of life for its members. While the opioid epidemic continues to affect communities across the nation, Centene remains committed to providing innovative programs, local support, and high-quality healthcare to every member.